
Intensive Outpatient Programs for Trauma in Ventura, CA
Traumatic experiences can impact a person’s nervous system, their relationships with others, and their daily activities. Yet, getting better doesn’t always mean staying in a hospital or stopping work or school. For many teens and adults, a trauma-focused Intensive Outpatient Program (IOP) offers the right balance of structure and flexibility for deep and sustainable healing.
In the following sections, we will explain how IOPs work for trauma, highlight research and clinical experiences regarding outcomes, identify who benefits the most, and outline what to expect if you choose a trauma-informed IOP at Channel Islands Mental Health Treatment.
What Is a Trauma-Focused IOP?
 An Intensive Outpatient Program (IOP) is a step up from regular weekly therapy but not as intense as programs like partial hospitalization or staying in a residential facility. Clients typically attend the program 3 to 5 days per week for a few hours each day, following a structured schedule that includes:
An Intensive Outpatient Program (IOP) is a step up from regular weekly therapy but not as intense as programs like partial hospitalization or staying in a residential facility. Clients typically attend the program 3 to 5 days per week for a few hours each day, following a structured schedule that includes:
- Individual therapy (e.g., EMDR, TF-CBT, CPT)
- Classes to learn new skills (such as DBT, emotion regulation, and distress tolerance)
- Psychoeducation (covering topics like the nervous system, triggers, sleep, and nutrition)
- Experiential and somatic therapies (including grounding, breathwork, and movement)
- Family sessions and care coordination, when appropriate
- Medication support, when clinically necessary
The goal of this program is to help alleviate symptoms, teach individuals to cope with distressing memories, and return to a normal life, allowing them to stay at home and apply what they have learned in everyday situations.
Why IOPs Are Effective for Trauma

2) Evidence-Based Modalities in One Place: Trauma IOPs bring together leading therapies like EMDR, Trauma-Focused CBT, Cognitive Processing Therapy, Prolonged Exposure Therapy, and DBT skills. This helps people receive care tailored to their specific needs, addressing both difficult memories and managing daily emotions.
3) Real-World Practice Between Sessions: Because clients live at home and keep going to school or work, they can use what they learn in everyday situations, like sticking to a sleep schedule, setting limits, and staying calm at work. This helps them remember and use these skills more widely.
4) Care Coordination & Family Involvement: Intensive outpatient programs offer doctor oversight, help manage your case, and family counseling when needed. Working together in this way is crucial for developing effective safety plans, preventing recurring problems, and fostering a supportive home life.
5)Step-Up / Step-Down Flexibility: IOPs can serve as a step-up from weekly therapy when symptoms worsen or as a step-down after inpatient or Partial Hospitalization Programs (PHP) to help maintain progress and reduce the risk of relapse.
Common Trauma Conditions Treated in IOP
- Post-Traumatic Stress Disorder (PTSD)
- Complex trauma / developmental trauma
- Trauma with co-occurring anxiety or depression
- Trauma-related dissociation (stabilization phase)
- Grief and loss related to traumatic events
- Trauma with co-occurring substance use (with integrated care)
What Progress Looks Like
Each person’s journey is different, but many people see significant improvements, which often include:
- Less panic, startle responses, insomnia, and irritability.
- Fewer flashbacks, nightmares, and ruminating thoughts.
- Better ability to manage emotions and tolerate distress.
- Improved focus and decision-making skills.
- Healthier relationships and clearer boundaries.
- A return to daily activities like school, work, and hobbies.
- A lower chance of going back to the hospital, with effective plans in place to prevent relapse.
What to Expect in a Trauma IOP at Channel Islands

- Comprehensive Intake and Goal Setting We begin by looking at your symptoms, past experiences, what you’re good at, and what sets you off. From this, we create a unique plan with three steps: stabilizing, working through issues, and reconnecting.
- Stabilization First Before working on any painful memories, we focus on building a strong foundation. We teach grounding techniques, sleep hygiene, nervous system awareness, and skills from Dialectical Behavior Therapy (DBT).
- Targeted Trauma Therapies When you’re prepared, we can begin specialized treatments designed for you. These could be EMDR, TF-CBT, CPT, or exposure therapy, all of which are backed by our effective methods for helping you feel stable.
- Somatic and Experiential Work We use gentle movement, breathwork, guided imagery, and mindfulness exercises to help your body complete its natural defenses and feel safe again.
- Skill Rehearsal and Homework You will receive short daily exercises that last about 5–15 minutes. These practices help reinforce what you learn and strengthen new connections in your brain.
- Family Engagement (When Helpful) When beneficial, we coach families to help them improve communication, establish limits, and react kindly to triggers.
- Medication Consultation If necessary, our psychiatric providers can help stabilize your symptoms and address any sleep issues you may be experiencing.
- Aftercare Plan Once you leave our program, we provide you with a comprehensive plan to help you stay well and avoid relapsing into old habits. This plan may include various options for ongoing support, such as weekly therapy, alumni groups, and virtual meetings.
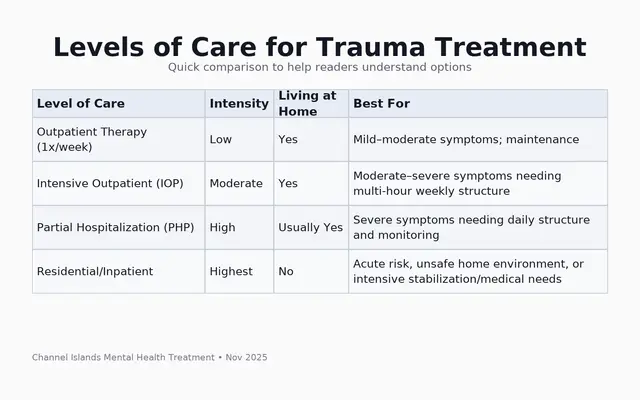
How IOP Compares to Other Levels of Care
Who Is a Good Candidate?

- Have PTSD or complex trauma that makes it hard to get through your daily life.
- Often face triggers that disrupt your day.
- Need more support than what you get from weekly therapy.
- Have recently moved from inpatient care or a Partial Hospitalization Program (PHP) and want to keep progressing.
- Deal with other issues like anxiety, depression, or trouble sleeping.
- Want to continue working or attending school while recovering.
What Helps IOPs Work So Well
- Phase-Oriented Treatment: This treatment follows three steps: Stabilization, Processing, and Integration. It helps you build coping skills before you deal with traumatic memories.
- Skills and Processing: Combining DBT skills with EMDR or TF-CBT helps reduce avoidance. This approach enables safe and gradual exposure to or reprocessing of traumatic experiences.
- Dose and Frequency: Going to multiple sessions each week helps you gain momentum. Spacing out sessions allows you to practice and apply the skills in real life.
- Collaborative Measurement: Regular check-ins on your symptoms enable your treatment team to adjust the plan, modify techniques as needed, and celebrate your progress.
Practical Benefits: Access, Cost, and Flexibility
- Live at home while keeping your routine.
- Evening and daytime sessions available based on your location.
- Assistance with work or school paperwork if needed.
- Most insurance plans are accepted; we’ll check your benefits before starting.
- Hybrid or telehealth sessions may be available, depending on state rules.
Tips for Choosing  the Right Trauma IOP
the Right Trauma IOP
- Ask what trauma therapies are available, such as EMDR, TF-CBT, CPT, PE, and DBT skills.
- Confirm whether psychiatric support and care coordination are available.
- Check for family involvement and aftercare plans.
- Ensure the program focuses on safety, choice, teamwork, trust, and empowerment.
- Talk about scheduling options that work for you.
- Request cost details and check your insurance benefits before you start.
Ready to Take the Next Step?
Channel Islands Mental Health Treatment provides a caring, trauma-focused program called Intensive Outpatient Program (IOP). This program helps you heal while you continue with your daily life. To learn more about our program and to request a private consultation, click here: Intensive Outpatient Program for Trauma.
Frequently Asked Questions (FAQ)
How long does a trauma IOP last?
Clients typically participate for 6 to 12 weeks, based on their individual goals and progress.
Can I work or go to school while in IOP?
Yes, you can. We help with scheduling and using new skills in everyday life.
Do you use EMDR?
Yes, our IOP includes EMDR and other effective treatments when appropriate.
What if I have panic attacks or feel disconnected?
We develop a safety plan that includes grounding techniques and gradual exposure to support you.
Is medication required?
Not always. Our psychiatric team will evaluate and prescribe medication only if it’s needed and agreed upon with you.
What happens after IOP?
You will get an aftercare plan, referrals for continued support, and strategies to prevent relapse.

 the Right Trauma IOP
the Right Trauma IOP